Introduction to Preclinical Research
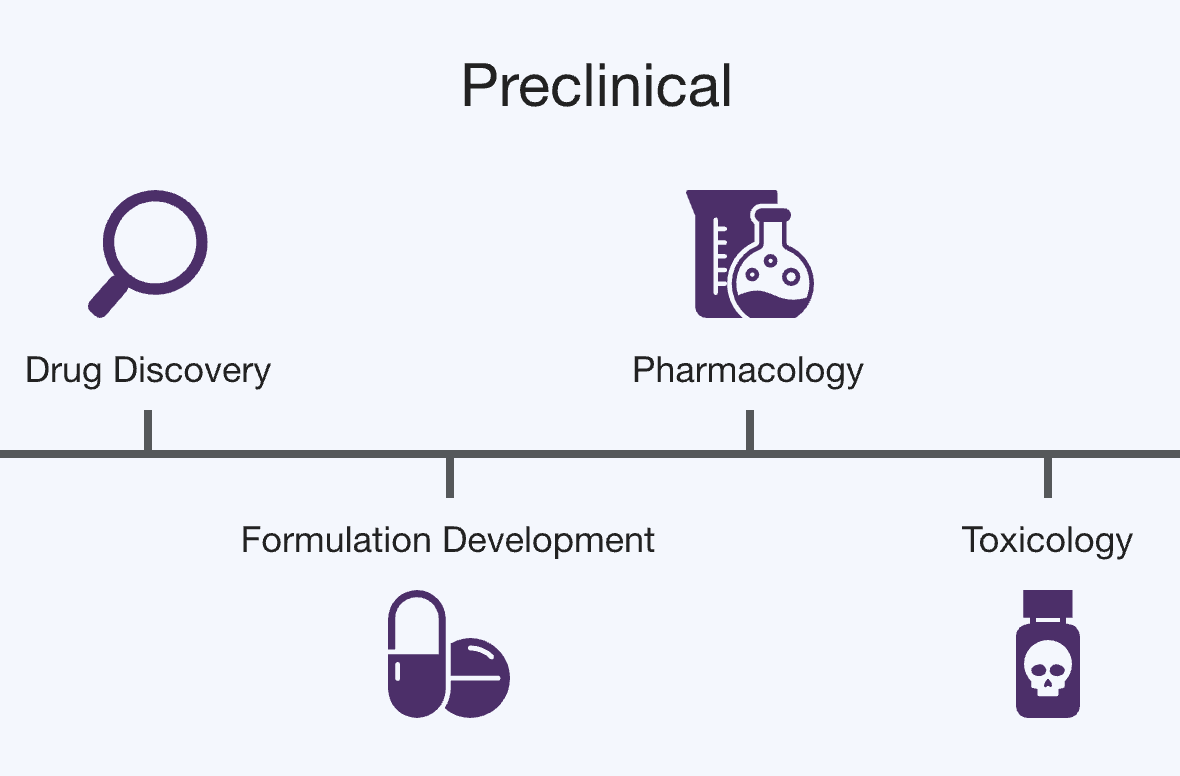
Preclinical research, often termed nonclinical, links discovery to first-in-human testing. Its purpose is to characterize pharmacology, toxicology, and pharmacokinetics to support dose selection and risk management before clinical trials. Activities span in vitro studies, in vivo animal studies under Good Laboratory Practice (GLP), and supporting analyses such as toxicokinetics and safety pharmacology. International expectations for what is required to begin and progress human studies are harmonized by ICH M3(R2) and implemented by regulators. (ICH Database, U.S. Food and Drug Administration, European Medicines Agency (EMA))
In the U.S. regulatory process, the FDA describes preclinical research as step 2 of drug development, focused on determining potential for serious harm and informing whether an Investigational New Drug application can proceed. The agency distinguishes in vitro and in vivo components and emphasizes toxicology. (U.S. Food and Drug Administration)
Typical study components
Common elements include general toxicity studies in at least two species, safety pharmacology, genotoxicity, local tolerance as relevant, and specialized studies depending on modality and indication. Study timing and duration are tied to the intended clinical exposure. (ICH Database)
Persistent scientific challenges
Translation from animals to humans
Outcomes in animal models often fail to predict human efficacy or safety. Systematic assessments report large variability in translational success, with only a small fraction of candidate interventions that show promise in animals ultimately reaching regulatory approval. Reported estimates include about 5 percent of therapies that progress from animal studies to regulatory approval after passing through human testing. The literature highlights model selection, outcome harmonization, and external validity as key determinants of translation. (PubMed Central, ScienceDirect)
Reproducibility and research rigor
Low reproducibility in preclinical work undermines cumulative knowledge and increases costs. Identified contributors include inadequate randomization and blinding, underpowered studies, and incomplete reporting. NIH and journal consortia have issued reporting principles and rigor frameworks to improve transparency. (PubMed Central, Grants.gov)
Variability and standardization under GLP constraints
Even with GLP processes, biological variability across strains, housing, and laboratory conditions can shift outcomes. Reviews stress the need for harmonized outcomes and detailed justifications for animal model choice to support external validity. (PubMed Central, MDPI)
Ethical and resource constraints
Efforts to reduce, refine, and replace animal use shape study design and may limit certain experiments. ICH M3(R2) explicitly aims to reduce unnecessary animal use through global harmonization and appropriate phasing of studies. (ICH Database)
Documentation to support regulatory decision making
Nonclinical packages must provide traceable, auditable evidence suitable for regulatory review, including study protocols, raw data, and analysis provenance that link results to human risk assessments. Guidance documents set expectations for when new studies are needed, for example when reformulating an approved drug or changing route of administration. (U.S. Food and Drug Administration)
The value of preclinical research is gated by translation, rigor, and documentation quality. Any methods, including AI, must be evaluated against these constraints and aligned to ICH and FDA expectations.